Chiropractic Care Through the Stages of a Woman’s Life
- Persistence Chiropractic Care
- Aug 27, 2025
- 11 min read
Updated: Sep 1, 2025
Because every woman deserves to feel cared for, at every stage of life.
Author: Pristencia Chow, Chiropractor
Women experience a wide range of physical, hormonal, and emotional changes throughout their lives. From puberty to postmenopause, each stage brings unique challenges and opportunities for support. Women face unique health challenges, from painful periods and hormonal shifts to chronic pelvic conditions. While conventional medicine offers a variety of treatments, more women are turning to chiropractic care as a natural, drug-free way to support their overall health and well-being. But what does science say?

Early Years: The Impact of Puberty
In the early years, puberty can be a confusing and overwhelming time. For some girls, it begins earlier than expected. Sometimes before age 10 which research links to increased risks of diabetes, obesity, heart disease and even breast cancer later in life. These early hormonal shifts may also lead to posture issues, growing pains, tension headaches, and mood changes. Rapid growth can cause misalignment in the spine and joints, often going unnoticed until discomfort appears. Chiropractic care during this stage helps support proper alignment, nervous system balance, and overall wellness—offering young women a healthy foundation as they develop.

Reproductive Years: Navigating Common Challenges
Between the late teens and late 30s, women often face a wide range of reproductive health challenges. PMS (premenstrual syndrome), painful periods, and hormonal imbalances can affect daily life, while conditions like PCOS, endometriosis, and fertility struggles can add emotional stress. Chiropractic care during this time can provide safe, drug-free relief from musculoskeletal tension, support pelvic alignment, and improve overall movement and energy. Many women find that consistent care helps regulate their cycle and reduce the intensity of PMS symptoms.

Menopause: Managing the Transition with Care
Menopause typically occurs between ages 45 and 55, bringing hormonal shifts that may result in weight gain, hot flashes, mood changes, sleep disruption, and joint stiffness. Estrogen also plays a key role in bone and joint health, and its decline can lead to increased pain, loss of flexibility, and decreased bone density. During this time, chiropractic adjustments can help manage stiffness, improve posture, reduce inflammation, and support the nervous system as the body adapts. Women often report better sleep, less joint pain, and improved mobility with regular care during this transition.
Postmenopausal Health: A Proactive Approach to Aging Well
In the postmenopausal years, women are at greater risk for conditions like osteoporosis, arthritis, and cognitive decline. While women generally live longer than men, they often experience more years with chronic pain or disability [4,6]. Taking a proactive approach to spinal health can make a significant difference in quality of life. Gentle chiropractic adjustments, movement therapy, and lifestyle coaching can help maintain mobility, reduce the risk of falls, and manage chronic discomfort [8]. At this stage, care is not just about treating pain—it's about preserving independence, strength, and confidence in everyday life.

How Chiropractic Care Supports Women at Every Stage?
Chiropractic care is more than just spinal adjustments. It's a whole-body approach rooted in the health of our nervous system. Across all stages of life, women may experience overlapping concerns such as fatigue, pain, sleep deprivation or fatigue. Chiropractic care helps regulate the stress response in our body, improve posture and movement, and support hormonal balance, all without medications or invasive procedures. Whether you're a teen adjusting to puberty, a new mom navigating postpartum recovery, or embracing your later years with strength, chiropractic can be a powerful part of your wellness journey. We’re here to help you feel aligned, balanced, and empowered. No matter your age or phase, do reach out to us to learn how chiropractic care can support your unique journey as a woman!
Some common conditions faced by women
Here’s a closer look at some of the most common women’s health concerns seen in chiropractic practice and what research reveals about their care.
Dysmenorrhea (Painful Periods)
Did you know that up to 90% of women of reproductive age experience menstrual cramps? For many, the pain isn’t just a monthly inconvenience, it can seriously interfere with daily life.
Understanding the Biomechanical Factors Behind Menstrual Pain:
Menstrual pain, known medically as dysmenorrhea, affects many women and can be divided into two main types: Primary and Secondary.
Primary Dysmenorrhea (PD)
This is the most common type and refers to crampy, recurring pain during menstruation without any underlying pelvic disease. The pain is often sharp and spasmodic, typically centered in the lower abdomen or suprapubic area. It can also radiate to the lower back or down the legs. Alongside the pain, many women experience mood swings, headaches, fatigue, nausea, and swelling. Symptoms usually begin a few hours before bleeding starts and may continue for a short time after.
Secondary Dysmenorrhea (SD)
This type is caused by underlying conditions such as pelvic inflammatory disease, endometriosis, or ovarian cysts. It typically develops a few years after menstruation begins. Factors like early onset of menstruation, higher body mass index, heavier or longer menstrual flow, smoking, and a family history of dysmenorrhea can increase the likelihood of developing SD. Stress and depression are also known to worsen menstrual pain [1].
What Causes the Pain?
Several biological mechanisms contribute to dysmenorrhea. Excessive contractions of the uterus, reduced blood flow to uterine tissues, and an increase in prostaglandin production all play a major role. Prostaglandins are natural chemicals released mainly within the first 48 hours of menstruation. They cause the uterus to contract and help expel menstrual blood, but when levels are too high, they can lead to intense cramping and discomfort. Prostaglandin causes pain that sends signals through nerves up to the brain. In some women, repeated pain signals can lead to central sensitization, where the nervous system becomes overly responsive. Hence, women often show irregular autonomic patterns including elevated sympathetic (fight or flight) activity and reduced parasympathetic (rest and digest) tone.
(Other compounds in the body also seem to influence menstrual pain. Elevated levels of vasopressin, a hormone that helps regulate water balance and blood pressure, have been found in women with PD. Similarly, nitric oxide and interleukin-6 play roles in inflammation and immune responses are often elevated. Research also shows that oxidative stress increases during menstruation, with higher levels of free radicals and signs of lipid peroxidation.)

Why does it matter to know the differences between PD & SD?
Understanding whether your pain is primary or secondary allows you and us chiropractor, as a primary healthcare provider to choose the right kind of treatment. Primary dysmenorrhea can often be managed with lifestyle changes and supportive care while secondary dysmenorrhea may require further medical evaluation to diagnose and treat the underlying condition.
Early recognition of chronic or worsening menstrual pain is important. Ignoring these symptoms may lead to increased nervous system sensitivity..
The good news is that there is growing research supporting natural ways to find relief. A study published in the Journal of Manipulative and Physiological Therapeutics found that women who received chiropractic spinal adjustments had a significant decrease in both menstrual pain and prostaglandin levels which are the natural chemicals that trigger cramping and inflammation. There is a randomized controlled trial that suggests chiropractic care may help calm the nervous system by releasing nerve interference and reduce the intensity of period pain [2]. This offers a drug-free option for women looking to feel better, naturally.
Premenstrual Syndrome (PMS)
Premenstrual syndrome, or PMS, affects many women, especially during the transition from adolescence to early adulthood. During this phase, the female hormonal system, known as the gonadal axis, is still developing. This system can be influenced by both internal and external factors, making it more vulnerable. This sensitivity may contribute to the onset of PMS, which presents with a range of physical, emotional, and behavioral symptoms.
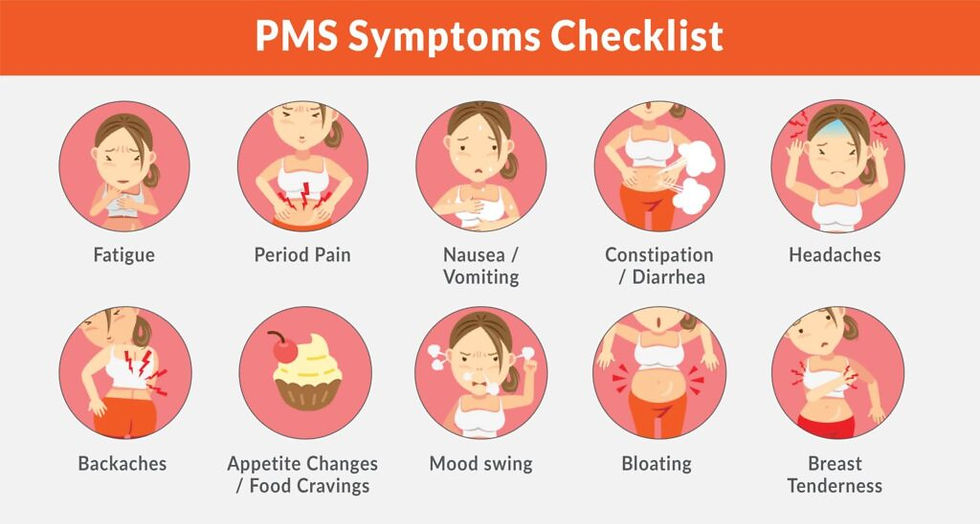
What Does PMS Feel Like?
PMS symptoms can differ from person to person, but they often fall into three main categories:
Emotional symptoms include low mood, anxiety, irritability, and a sense of losing control.
Behavioral symptoms may involve changes in appetite, difficulty sleeping, and withdrawal from social activities.
Physical symptoms can include headaches, breast tenderness, bloating, fatigue, and digestive discomfort such as diarrhea.
These symptoms tend to appear in the days leading up to menstruation and can interfere with daily routines and overall well-being.
Why Does PMS Happen?
While PMS has long been associated with changes in estrogen and progesterone levels, hormone fluctuations alone do not explain all cases. Many women with PMS do not have abnormal hormone levels. This has led researchers to look at other contributing factors such as:
Body mass index
Socioeconomic background
Age at first menstruation
Personality traits including emotional sensitivity and anxiety
History of trauma, particularly during childhood
All of these elements combine to form a more complete understanding of what causes PMS.
Nervous System and Stress Response - The autonomic nervous system, which manages automatic functions such as heart rate and digestion, may also be affected. Women with PMS may experience a shift toward increased stress activity and reduced relaxation, making the body more reactive to pain and emotional triggers.
The Role of Inflammation and the Immune System - The body treats menstruation as an inflammatory process. Chemicals such as prostaglandins and cytokines are released to help shed the uterine lining. While necessary, these substances can also cause bloating, cramping, and mood changes. Women with PMS may have a stronger-than-usual inflammatory response or elevated levels of oxidative stress, which can make symptoms more intense.
Hormonal Sensitivity and Mood Changes - During a typical menstrual cycle, estrogen and progesterone levels drop sharply just before a period begins. This hormonal shift impacts brain chemistry. One substance, allopregnanolone, is a byproduct of progesterone and usually promotes calmness by interacting with GABA receptors in the brain. In some women, this calming effect is reduced or disrupted, which may lead to increased anxiety, irritability, or emotional shifts before menstruation.
Brain Chemistry and Emotional Regulation - Brain chemicals like serotonin and GABA are closely connected to PMS symptoms. When estrogen levels fall, serotonin levels can also decrease, which may lead to mood swings, cravings, and trouble sleeping. In addition, changes in how the brain reacts to progesterone and its related compounds may heighten anxiety or emotional sensitivity. Some studies have also shown that areas of the brain responsible for regulating stress and emotions may behave differently during the menstrual cycle in women with PMS [10].
Nutrition and Genetics Matter Too The body needs key vitamins and minerals to support hormone balance and nervous system health. Low levels of magnesium, calcium, vitamin B6, and vitamin E have all been linked to more severe PMS symptoms. Genetics can also influence how sensitive a woman is to hormone changes or how her body responds to inflammation. Lifestyle factors such as lack of sleep, high stress levels, and limited physical activity can further aggravate symptoms.
While chiropractic care focuses on the spine and nervous system, both of which play important roles in hormonal balance, muscle tension, and the body stress response. So, how does chiropractic care adjustments help with PMS?
Chiropractic & PMS - Here is How:
Balancing the autonomic nervous system, helping regulate hormonal fluctuations and stress levels.
Reducing spinal and pelvic tension, improving mobility and reducing cramping.
Improving circulation and lymphatic flow, potentially easing bloating and fatigue.
Eases musculoskeletal pain, especially in the lower back and hips.
While more research is needed, these results indicate that chiropractic adjustments may help balance the autonomic nervous system and support hormonal health during the menstrual cycle. PMS is not just a minor inconvenience. With the right support and guidance, women can manage symptoms more effectively and improve their overall quality of life.

Chronic Pelvic Pain
Chronic pelvic pain (CPP) affects up to 20% of women worldwide and remains one of the most complex and often misunderstood women’s health concerns. While it is commonly linked to gynecological conditions such as Endometriosis, scientific research reveals that chronic pelvic pain often involves a wide range of biomedical factors [7]. These include inflammation, nerve irritation, muscle imbalances, and changes in how the nervous system processes pain.
In this post, we will explore the major biomedical contributors to chronic pelvic pain and how they may affect a woman’s daily life and long term well-being.
Nervous System Sensitization
Over time, repeated pain signals can cause the central nervous system to become more sensitive. This phenomenon is known as central sensitization. It can lead to heightened pain responses, even in areas where there is no ongoing injury. Women with this condition may feel persistent discomfort not only in the pelvis but also in other parts of the body. This heightened sensitivity can remain even after the original cause of the pain has been treated.
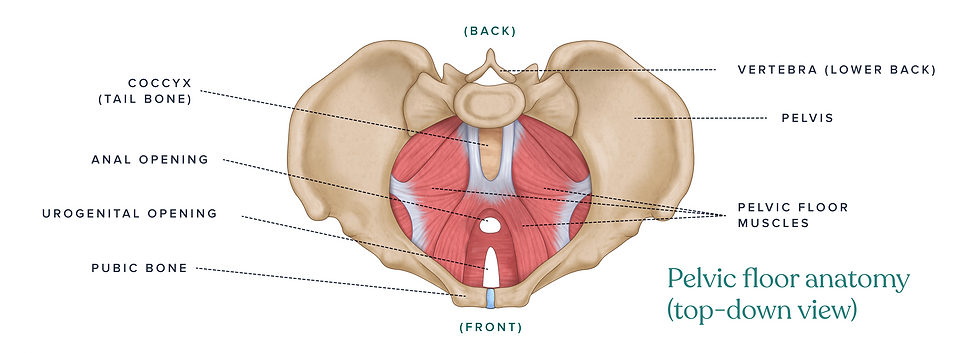
Pelvic Floor and Musculoskeletal Dysfunction
Pelvic floor muscles support the organs in the lower abdomen. If these muscles become too tight, weak, or unbalanced, they may contribute to long-term pelvic pain. This discomfort often increases with stress, physical activity, or prolonged sitting. In some cases, nerve entrapment such as pudendal neuralgia can cause burning, tingling, or aching sensations due to irritation of nerves in the pelvic region.
Inflammation and Endometriosis
Endometriosis is one of the most well-known causes of chronic pelvic pain. In this condition, tissue that resembles the lining of the uterus grows outside of it. This tissue can produce inflammatory substances that irritate surrounding nerves, increasing pain sensitivity. Many women experience cramping, deep pelvic pain, and discomfort that radiates to the lower back or legs [11].
Organ Involvement
Pain may also come from conditions like painful bladder syndrome, irritable bowel syndrome, or ovarian cysts. These can mimic musculoskeletal pain and often overlap, making diagnosis complex [12].
Connective Tissue and Hormones
Conditions affecting muscles and ligaments, along with hormonal shifts during menstruation, pregnancy, or menopause, can reduce pelvic stability and increase pain sensitivity [11].
Mind-Body Connection
Stress, anxiety, and past trauma can amplify pain. Addressing emotional health is essential in chronic pain management.
Chiropractic Care for chronic pelvic pain
Because chronic pelvic pain involves many systems of the body, care must be comprehensive and personalized. In chiropractic practice, we focus on improving spinal and pelvic alignment, relieving nerve interference, muscle tension, and restoring mobility. We may also collaborate with pelvic floor physical therapists and other healthcare providers to offer complete support.
Women living with chronic pelvic pain deserve to be heard and supported. With the right approach and a caring team, lasting relief is possible.
Conclusion
Women’s health is a dynamic journey that deserves attention and care at every stage. By understanding the unique challenges and opportunities that arise, women can empower themselves to lead healthier and happier lives.
What ties these conditions together is the role of the nervous system and musculoskeletal alignment in how the body functions and feels. Chiropractic care focuses on optimizing spinal health, which in turn helps relieve nerve interference, regulate pain signals, hormonal balance, mental clarity and mobility.
In a time when many women are seeking holistic and preventative approaches, chiropractic provides a valuable complement to traditional medical treatment.
Hence, this is why encouragement of integrating chiropractic care into your wellness routine may be just what you need to support your journey as women and human.

Reference:
Goerl K, Hensel K, Dusek J, et al. The Effect of Chiropractic Care on Menstrual Pain: A Systematic Review and Meta-Analysis. J Manipulative Physiol Ther. 2019;42(9):629-638.
Lee JH, Choi TY, Lee MS, et al. The Effect of Chiropractic Care on Pregnancy-Related Low Back Pain: A Systematic Review. J Altern Complement Med. 2017;23(2):98-106.
Buchan J, Houghton A, Macfarlane GJ, et al. The relationship between menopause and musculoskeletal pain in women: a systematic review. Menopause. 2010;17(1):119-127.
Haas M, Kuo T, Kwan M, et al. Osteoporosis in Women: A Review of the Role of Chiropractic in the Prevention and Treatment. Chiropr Osteopat. 2009;17:5.
Rees MA, Evans A, Harden A. Understanding women's health information needs for decision-making across the lifespan: A scoping review. Patient Educ Couns. 2019;102(8):1350–64.
Mirtz TA, Thompson MA. Osteoporosis and osteopenia in premenopausal women: A review of risk factors and management considerations for the chiropractor. J Contemp Chiropr. 2022;5:204–9.
Juzych NS, Chopra S. Women's Health Issues. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
Nedelec L. Preventive Health Care for Women. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
Alcantara J, Lamont AE, Ohm J, Alcantara JD. The safety and effectiveness of pediatric chiropractic: A survey of chiropractors and parents in a practice-based research network. Explore (NY). 2019;15(5):386–94.
Rode MV, Kamble P, Phatak MS, Jadhao P, Tayde P. Effect of premenstrual stress on autonomic function. Ann Neurosci. 2010;17(3):131-3. doi:10.5214/ans.0972-7531.1017307
Bajaj P, Bajaj P, Madsen H, Arendt-Nielsen L. Endometriosis is associated with central sensitization: a psychophysical controlled study. J Pain. 2003;4(7):372-80. doi:10.1016/S1526-5900(03)00720-X. PMID:14622679.
Hoffman D. Central and peripheral pain generators in women with chronic pelvic pain: patient centered assessment and treatment. Curr Rheumatol Rev. 2015;11(2):146–66. doi:10.2174/1573397111666150619094524. PMID:26088216.







Comments